Improving Nurse Rounding Programs with RTLS Enabled Solutions

Tony Natale, Director of Strategic Partnerships
“Trust, but verify” is a Russian proverb made famous by Ronald Reagan back during the late days of the Cold War. The expression came to mind as I was puzzling over HCAHPS scores and how a well-executed nurse rounding program can positively impact patient satisfaction – and yet I still see so many hospitals continuing to perform poorly.
The negative financial effect of poor HCAHPS scores on hospital reimbursement is widely recognized by those in the healthcare community. For larger hospitals, millions of dollars of reimbursement incentives from the Centers for Medicare and Medicaid Services (CMS) are contingent upon the Value Based Purchasing (VBP) program. A hospital’s Total Performance Score (TPS), of which HCAHPS results are a significant contributor, is the basis of each hospital’s reimbursement incentive adjustment.
The dimension of the HCAHPS survey with the highest correlation to its “Overall Hospital Ranking” is “Communication with Nurses.” Press Ganey looked into these correlations even more deeply and discovered that 5 HCAHPS dimensions - nurse communication, staff responsiveness, pain management, communication about medicine and total score - had a clustering effect where these measures consistently hang together. This cluster will have a 15% impact on a hospital’s VBP score. Obviously, high performance is very important in these dimensions.
If you look closely at those five dimensions it is fairly easy to see that nurse rounding could help in all of those areas. In fact, most nurse rounding protocols use some variation of the “3P’s” (or 4 or 5) - pain, potty, and position - for their purposeful hourly rounding programs. A C-Level hospital executive once said to me “Every time a patient rings the call bell it is a chance for us to fail.” A cynical view for sure. However, it seems logical and the data bears out that if staff is regularly in the patient’s room asking about their needs they are lowering demand for patient calls.
Every hospital I have visited in the last three years has implemented a nurse rounding program. Every single one. And I have been in dozens and I have asked. What I can’t always tell is whether they are executing it well. How are they documenting the rounding? Are they doing a good job of rounding on time every hour or 2 hours? Are they compiling and analyzing the historical data? How do they know in real time when rounding is due or if rounding has been missed?
An entire industry has sprung up around helping hospitals with their rounding programs. There are consulting firms that help set up the protocols and train the staff. There are paper-based rounding log forms. There are IT-based solutions in the form of apps for smart phones and tablets that help enable and document the rounding process. The nurse call manufacturers have rolled out optional wall mounted touch screens that allow caregivers to acknowledge rounding events and re-start timers. All of these tools are great and can be used alone or in some combination with each other.
So why is it still so common for me to find hospitals whose VPB scores continue to decrease, year after year, when there is a proven rounding solution and there are obviously many tools and resources available to help? The challenge that I have witnessed time and time again is that, on their own, each of the tools above require the caregiver to DO something. Whether it’s to write something down or touch a screen of some sort. The minute a human being has to take the initiative to acknowledge that rounding is complete or initiate the next cycle is the minute that the system can break.
“No one can sabotage a healthcare technology deployment faster than a staff nurse.” – Linda Groah, CEO/executive director of AORN.
So, what is the missing ingredient? Real-time locating system (RTLS) technology.
RTLS eliminates the need for staff to interact with the rounding compliance system and CenTrak’s Clinical Grade™ locating technology lives entirely in the background. Caregivers wear CenTrak’s RTLS staff badge behind their other ID badges and the system automatically detects when the caregiver has entered the room, as well as the length of time spent with each patient. Only CenTrak RTLS offers the certainty-based accuracy required to do this effectively.
Another unique RTLS-enabled feature is that the system is proactive. A visual floor plan of the nursing unit is displayed on a large screen at the nurse’s station (or other strategic location) to remind nurses when rounding is due or overdue on a particular room. Customizable reports let managers and executives review compliance and historical performance. Integrations with wireless devices and software applications from CenTrak’s partners allow more options for proactive rounding reminders.
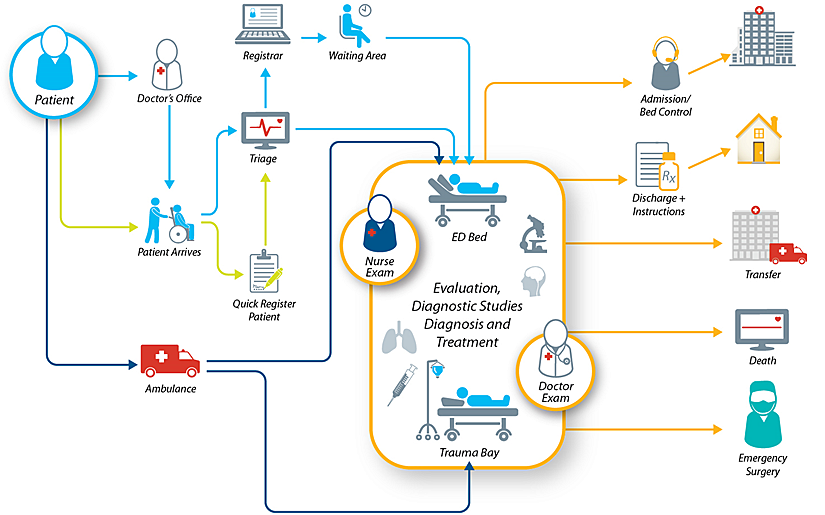
The benefit of nurse rounding is obvious. Executing well is critical. Nurses need to be able to focus on providing excellent care which is why CenTrak’s proactive RTLS technology does not require staff interaction with the system. Additionally, an investment in CenTrak's RTLS enabled nurse rounding solution can also be leveraged for hand hygiene compliance, asset tracking/management, patient workflow improvement, temperature/environmental monitoring, infant security and many other uses that improve patient care and hospital operations.
Trust, but verify.